PCOS Causes and How to Heal PCOS Naturally
Table of Contents
What is PCOS?
What defines PCOS for diagnosis
How is PCOS diagnosed?
Understanding hallmarks of PCOS: Cysts, Irregular cycles, Androgens.
PCOS Symptom checklist
Is PCOS genetic?
The 6 causes of PCOS
Foods for PCOS
Introduction
PCOS is a hormonal disorder affecting millions of women around the world. The exact cause of PCOS is unknown, and it is theorized that different issues within the body could influence the manifestation of PCOS. PCOS is influenced by genetics, environment, nutrition, and the functional health of your whole body (1). Improving your nutrition and overall health can have a ripple effect of positive improvements in your PCOS.
What is PCOS?
PCOS stands for Polycystic Ovarian Syndrome. The keyword here is syndrome.
A syndrome is “a condition characterized by a group of symptoms that consistently occur together.”
In other words, we don’t why it happens, but it happens often enough to give it a name!
1 in every 10 women have PCOS but many women go years before receiving the diagnosis (2). One of the reasons for this is that the symptoms vary person to person. You and your best friend can both have PCOS and each have a different set of visible symptoms. Some of the symptoms of PCOS like weight gain, acne, and irregular periods may even be dismissed as “normal,” further delaying an accurate diagnosis.
What defines PCOS for diagnosis?
There are two sets of criteria for diagnosing PCOS. The Rotterdam criteria and the Androgen Excess and PCOS Society Criteria.
The Rotterdam Criteria
If your doctor uses the Rotterdam Criteria, there are 3 big signs they will check when investigating a PCOS diagnosis (3).
Multiple cysts on your ovaries
High levels of blood androgens (testosterone)
Irregular periods
You need two of these signs for a doctor to consider a PCOS diagnosis. Any combination can get you a PCOS diagnosis.
It is entirely possible to have elevated blood androgens and irregular period, but no cysts show up on an ultrasound. This also means a doctor will not diagnose PCOS on ultrasound findings alone.
Having multiple cysts does not necessarily indicate that you have the condition.
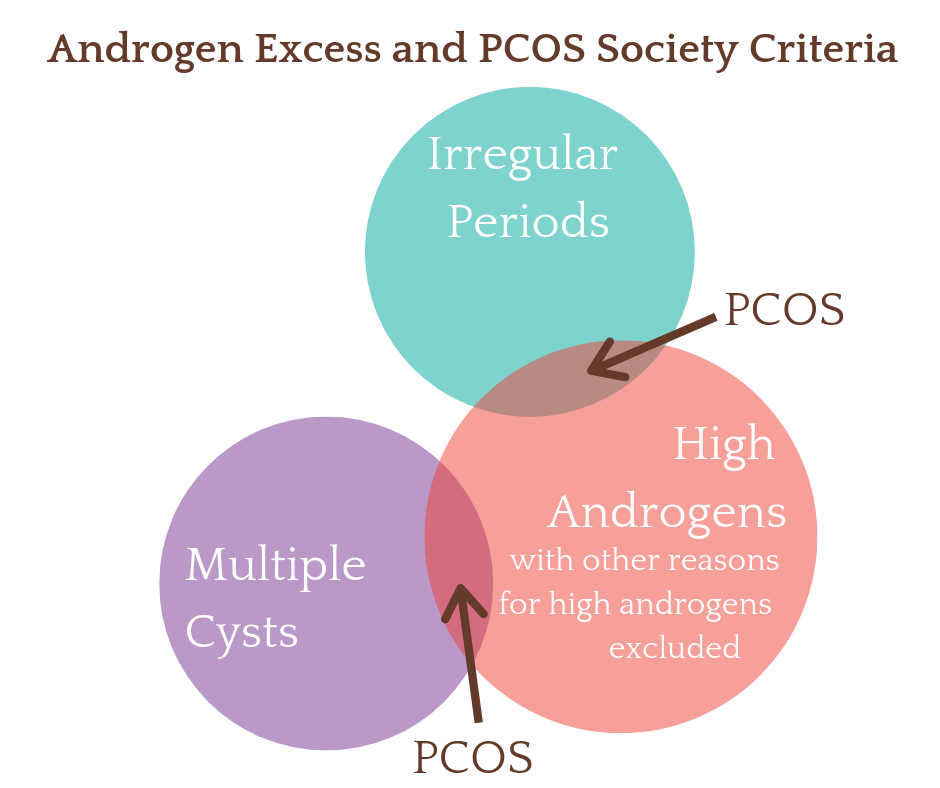
The Androgen Excess and PCOS Society Criteria
This criteria requires the presence of excess androgens as a diagnostic criteria (4). You must have all three of these criteria to get a PCOS diagnosis.
Excess androgens in a blood test.
Other reasons for excess androgens have been excluded.
Ovarian dysfunction (not ovulating) or polycystic ovaries.
This set of criteria differs from the above Rotterdam Criteria by requiring the presence of excess androgens for a diagnosis of true PCOS. For example, with the more general Rotterdam criteria you could receive a PCOS diagnosis with multiple cysts and irregular cycles only. There are many other reasons those two symptoms could occur together that are not linked with PCOS.
For example, a teenager who is producing 25 follicles per month and who is under emotional stress from exams and physical stress from competitive sports could certainly have a few anovulatory cycles and have multiple cysts visible on an ultrasound. However, her scenario is likely temporary and not indicative of true PCOS.
How is PCOS diagnosed?
Blood Tests
Excess androgens is one of the hallmarks of PCOS. But it is not something you can observe. Your doctor will order a blood test in order to determine your levels. They likely will also test your other hormones. Always get a copy of your lab results for your personal records. It is helpful to keep this information in one place and monitor your progress over time. There are many doctors and practitioners who can help you manage your PCOS, and you are ultimately the one in control of your own health.
Common blood test your doctor might order:
Free testosterone - Less than 4% of total testosterone circulates as free, bioavailable testosterone. This is considered the best test for identifying a condition (5).
Total testosterone - This tests for the total quantity of testosterone in the blood. It does not show how much of the testosterone is circulating freely and how much is bound to SHBG. It is helpful to also test for SHBG if testing total testosterone to get a clearer picture. SHBG may be low in women with PCOS (6).
SHBG (Sex Hormone Binding Globulin) - SHBG binds to both testosterone and estrogen and transports the inactive forms of these hormones through the blood stream.
Androstenedione - Androstenedione is produced by the ovaries and the adrenal glands. It is a precursor (building block) to make testosterone and estrogen. Androstenedione may be higher in women with PCOS (7).
DHEA-S - DHEA-S is the sulfated version of DHEA. This means the molecule DHEA has a sulfur group attached to it, which makes it inactive. A test for DHEA itself is an indicator of the body’s response to an immediate stressor and the test for DHEA-S is a better indicator of the body’s total, life-long storage level of DHEA (8). DHEA-S is produced exclusively in the adrenal glands (9).
Ultrasound
PCOS cannot be diagnosed by ultrasound alone (10). An ultrasound is used to see the multiple cysts that PCOS is named for. It will look like a string of pearls around the edge of your ovary. It is possible to have PCOS and not find cysts on an ultrasound. And it is possible to find multiple cysts and not have PCOS. Due to the nature of the menstrual cycle (it is always changing!) the ultrasound will look different every month.
Cycle Charting
Irregular cycles are very common among women in general. While it is common - it is not ideal. Tracking your monthly cycle is the best way to get a clear picture of your hormonal health.
At minimum, track the length of your period and overall cycle length.
If you suspect a hormonal imbalance or are trying to become pregnant with PCOS, consider tracking cervical mucus and basal body temperature in addition to your period and cycle length. This will give you a far clearer picture of your hormonal health.
Understanding the 3 Hallmarks of PCOS: Cysts, Irregular cycles, and Androgens.
How do multiple cysts form in PCOS?
Each month Follicle Stimulating Hormone (FSH) stimulates the ovaries to develop follicles. Each follicle contains an immature egg. What’s supposed to happen is that the follicle grows, the egg matures, signals are sent from the ovary to the pituitary saying that the egg is ready. The pituitary responds with hormones that trigger ovulation. The follicle releases the egg during ovulation, then the follicle transforms into a corpus luteum which begins producing progesterone.
In a woman with PCOS these follicles stop developing. The result is that the hormonal signaling that tells the pituitary the egg is ready are not sent, and so ovulation does not occur. The underdeveloped follicles go on to become small cysts which are eventually reabsorbed. If you have an ultrasound done in the later part of your cycle, you may be able to see these cysts. They look like a string of pearls on the side of your ovary.
2. Why do women with PCOS have irregular periods?
First, it’s important to know what a normal cycle looks like for you. The 28 day cycle is a myth. Anywhere between 26-33 days is healthy. It’s important to monitor your own cycle to know what is regular for you. For example, if you cycle is usually 29 days and suddenly it’s 33 days, that is irregular for you, even though 33 days is a healthy cycle length.
Women with PCOS often have very long cycles, over 33 days, or skip periods completely.
It is often the lack of ovulation that causes irregular cycles. The body will wait a few extra days for ovulation to occur. When ovulation doesn’t happen, eventually you will menstruate but your cycle has already been extended by a few days or weeks.
High testosterone levels can also make it hard for your body to menstruate. This can make your cycle even longer.
3. What causes increased androgens?
The ovaries naturally produce a small amount of androgens. This is perfectly normal and healthy. Androgens help increase libido and mood. But when androgen levels are too high they create negative side effects.
Androgens include testosterone, DHEAS (the combination of DHEA and DHEA-S), and androstenedione.
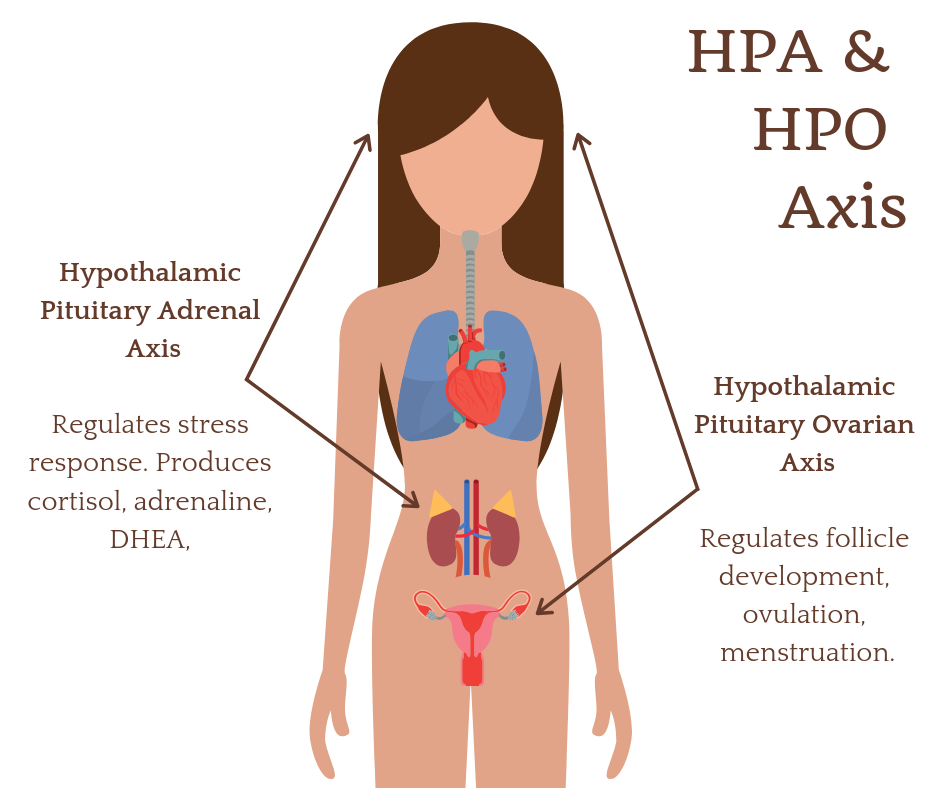
Androgens are produced in the ovaries and adrenal glands. It’s important to remember that these endocrine glands, the ovaries and adrenals, do not act on their own free will. They act in response to direction from the pituitary gland. These organs function through feedback loops that are finely tuned based on functions throughout the entire body. There are multiple reasons androgens can increase, including chronic stress, insulin resistance, use of hormonal birth control, and chronic inflammation. It is important to take a whole-body approach and seek the root cause when managing PCOS.
PCOS Symptom Checklist
This is a full list of symptoms linked with PCOS. You will not have all of these symptoms because PCOS is not one disease with one cause. PCOS is a set of symptoms that often occur together. PCOS could result from insulin resistance, adrenal dysfunction, thyroid dysfunction, extreme stress, chronic inflammation, or coming off the hormonal contraceptive pill.
The more items on this list you check off, the more likely it is that you have PCOS. Your symptoms can also give you a clue about which issue might be the root cause of your PCOS.
Symptoms of Excess Androgens
Excess hair growth on your face, arms, back, and chest.
Thinning hair on your head, also known as male pattern baldness
Acne
Headaches
Painful bumps under the skin (Hidradenitis Suppurativa) usually around the armpit or groin.
Symptoms of Insulin Resistance (linked to 70% of PCOS cases)
Weight Gain & difficulty losing weight
Trouble Sleeping, including waking in the middle of the night and having trouble getting back to sleep.
Darkened skin, especially around neck (Acanthosis Nigricans)
Skin tags
Low sex drive
Hypertension
Symptoms of Irregular cycles & lack of ovulation (anovulation)
Infertility, trying to become pregnant without success for a year.
Irregular Periods that change length month to month or are consistently very long, this also includes skipped and missing periods.
Heavy Periods can be an indicator.
Using at home Ovulation Predictor Kit and not getting a positive in between cycles.
Other symptoms
Being underweight, this is a subset of women who experience PCOS due to undereating and over exercising.
Chronic Stress, this includes physical stress like over exercising or emotional and psychological stress.
Digestive symptoms are worth paying attention to
Running cold, especially having cold hands and feet
Recent use of hormonal birth control (the Pill).
Is PCOS Genetic?
Studies have shown that you are more likely to have PCOS if someone in your family also has PCOS. However, genetics are unlikely to be the cause of your PCOS.
Genes load the gun and environment pulls the trigger. This means that if you have a predisposition toward insulin resistance and if you combine that with a diet high in processed food, refined carbohydrate, and not enough nutrients, then your result will be PCOS.
The good news is that genes are only one part of the equation! Supporting the other half, your environment (lifestyle, exercise, food) can dramatically reduce the likelyhood of PCOS or complications from it.
So if genes don’t cause PCOS, what does?
The 6 Causes of PCOS
#1 Insulin Resistance
In fact it’s estimated that 70% of PCOS cases have a root cause in insulin resistance. Insulin resistance means that your cells have stopped listening to the messages of insulin, they’ve become resistant, and so your body makes even more insulin in response. It’s like talking through a megaphone to force the cells to listen. Insulin resistance could be caused by too much sugar and refined carbohydrates in the diet, or it could be caused by chronic inflammation. In either case, research has shown that high levels of insulin directly stimulate the ovaries to produce more testosterone than they should. High testosterone, and other androgens, is a hallmark of PCOS.
Key Nutrients to heal insulin Resistance:
Ditch sugar! This is step number one. Even the best supplements in the world can’t make up for a diet high in sugar and refined carbs.
Minerals: Chromium and magnesium are two crucial minerals needed for your body to keep your energy stable in between meals.
B Vitamins: The B vitamins play an important role inside your cells by helping the cells turn glucose into usable energy, called ATP.
#2 Coming off the pill
It can take a few months for your body to recalibrate after coming off the pill, sometimes 1 month for every year you were taking synthetic hormones. It’s not uncommon to see insulin resistance and excess androgens during this time which a doctor might qualify you for a PCOS diagnosis. In this case, your body will likely come back into balance on it’s own. However, if you went on the pill because of irregular period, whatever problem you had before you started the pill will still be there when you come off, so it’s important to work on overall health to support your body through this transition.
Nutrients to support hormones after coming off the HBC pill
B vitamins are quickly depleted while using hormonal birth control. Getting plenty of B vitamins will help your body recover faster.
Minerals: Zinc, Magnesium, and Selenium are also depleted while using hormonal birth control. Minerals are like the spark plugs in the body. Focusing on mineral rich foods will provide your body with important minerals to create enzymes needed for energy production.
#3 Hypothyroid PCOS
Your thyroid is a butterfly shaped gland on your neck that produces the hormone T3. T3 is required by all cells in order to function properly, including the follicular cells in your ovaries. In some women, a lack of T3 could be causing the multiple cysts on her ovaries. Remember, multiple cysts on it’s own is not sufficient for a PCOS diagnosis. In this case hypofunctioning thyroid and low T3 may be one piece of your PCOS puzzle. There are many steps in the process of creating T3, any one of which could go wrong. If you suspect that low functioning thyroid is a part of your PCOS story, be sure to have a full thyroid panel run, including the test for Hashimoto's Thyroid Antibodies to rule out an autoimmune condition.
Nutrients to Support the thyroid
Iodine is a critical nutrient for healthy thyroid. Your thyroid needs iodine in order to produce thyroid hormones T3 and T4. If you suspect thyroid dysfunction, have your TPO antibodies checked by your doctor. TPO antibodies indicate an autoimmune thyroid condition. Use great caution and always work with a skilled clinician when attempting to supplement iodine with a thyroid condition.
Gut healing: It seems counter intuitive that digestion and thyroid health are related, but they are! Poor digestion creates inflammation in the body, allows pathogenic microbes into the blood stream, overstimulates the immune system, and puts unnecessary stress on the liver. All of these issues can lead to a perfect storm that ends in thyroid dysfunction and PCOS. Adding healing nutrients can soothe the gut and calm the immune system. Supplementing with herbs like licorice, marshmallow root (not marshmallows from the store!), okra, and aloe vera can provide healing nutrients to calm an inflammed digestive tract.
#4 Inflammatory PCOS
If you have ruled out the other types of PCOS so far and you have signs of chronic inflammation in your body such as joint pain, eczema, psoriasis, headaches, or chronic digestive issues, inflammation may be playing a part in your PCOS. It is important to work with someone who can help find the cause of your inflammation and take steps to support the body’s natural anti-inflammatory processes.
Nutrients to calm inflammation
Gut healing: Supplementing with herbs like licorice, marshmallow root (not marshmallows from the store!), okra, and aloe vera can provide healing nutrients to calm an inflammed digestive tract. Collagen also contains gut healing benefits. You can add collagen into your day by sipping a cup of homemade bone broth or adding scoop of Vital Proteins Collagen Peptides to your morning decaf coffee.
Omega-3s: Healthy fats, specifically omega-3s, are used to fuel the body’s natural anti-inflammatory processes. Simply being deficient in omega-3s can prevent the body from being capable of calming inflammation on it’s own! Adding an extra serving of wild caught seafood each week is a great way to get omega-3s in your diet. I also love to keep a bottle of La Tourangelle’s Nutri-blend oil on hand to use on salads. It’s a blend of organic sunflower, sacha-inchi, coconut, and sesame seed oils and is super high in omega-3s!
#5 Adrenal PCOS
One of the hallmarks of PCOS is high blood androgens. If you have normal levels of ovarian androgens like Testosterone, but high levels of DHEAS, an androgen produced in your adrenal gland, this may be your root cause. If this is the case, you are likely in a chronic stress response. Your internal operating system has two modes - sympathetic, fight or flight, and parasympathetic, rest and digest. Part of your healing journey is going to include working with someone who can help your body learn to switch modes more easily so you aren’t stuck in fight or flight all day.
Nutrients to support adrenals
First, always address the source of stress. Practicing mindfulness, meditation, journaling, life coaching, and therapy are all great ways to reduce stress.
Adaptogenic herbs: Adaptogens help bring the body into balance. If your adrenals are on overdrive, adaptogens calm them. If your adrenals are exhausted (or not communicating correctly with the hypothalamus), adaptogens give them a boost. Holy Basil, also called Tulsi, ashwaganda, and rhodiola are fantastic adaptogens for the adrenals. The herbal tinctures from Wise Woman Herbals are a great way to use adaptogens.
#6 Extreme Stress PCOS
Extreme physical stress that can cause PCOS involves dieting, rapid weight loss beyond what is healthy for that individual, and a regimen of vigorous exercise. In many cases this will create a condition called hypothalamic amenorrhea where your period disappears. Your body believes it is experiencing starvation. Hormone levels will decrease, you’ll lose your period, and in some women your testosterone might stay at the same level, while everything else decreases or it might rise, causing the excess androgens that a doctor would look for in a PCOS diagnosis. Even if your hypothalamic amenorrhea triggers PCOS, the pattern of dieting, calorie restriction, and extreme exercise must be addressed first. Seek out a doctor or practitioner who is familiar with this condition and who can support your physical, mental, and emotional needs.
Extreme stress can also be psychological. You can be at home, perfectly safe, and create a stress response in your body through the images we play in our minds. Worrying is stress, negative self talk is stress, reliving past events is stress. A habit of stressful thinking can create the same stress response in our body as though we were being chased by a tiger. It is very real and is something we’re all affected by. The good news is you can recondition your thought patterns and manage the mental chatter in your head to reduce stress. I’ll link to a great resource for this in the video description.
Nutrients to heal after extreme stress
After being in a state of extreme stress it’s valuable to work with a practitioner who can assess your body’s current needs. Some women may need calming nutrients like calcium, magnesium, and adaptogens. Others may need slightly stimulating nutrients. The goal with nutritional therapy is to bring the body into balance. Especially after an episode of extreme stress, it’s best to test - not guess about what your body needs right now.
Nutrient density: Focusing on nutrient dense foods is always a good idea. You may find that soups and stews are easy to prepare and easy to digest as your body heals.
Foods for PCOS
The best thing you can do for your PCOS is to eat real, whole foods.
Don’t tune out if you’ve heard that before!!
More information isn’t always what you need. You need to eat better food. You need to improve your bad eating habits. This is how you improve your PCOS.
Healthy Carbohydrates for PCOS
Studies have shown that lower carbohydrate diets can improve PCOS. However, a low carb diet is NOT a no carb diet. Focus on getting carbohydrates from vegetables and you’ll receive all the benefits of healthy carbohydrates without the negative affects of processed, refined carbohydrates.
Eat abundant amounts of the following veggies!
Artichoke
Asparagus
Beet
Bell Pepper
Broccoli
Brussels sprouts
Cabbage
Carrot
Cauliflower
Celery
Collard Greens
Cucumber
Eggplant
Endive
Frisee
Green beans
Jalapeno
Jicama
Kale
Kohlrabi
Leek
Lettuce
Mushrooms
Okra
Onion
Parsnip
Peas
Radicchio
Radish
Rutabaga
Snap peas
Spaghetti squash
Spinach
Summer Squash
Tomato
Turnip
Zucchini
Eat moderate amounts of the following starches. For example, 1/4 cup of cooked grains in your salad for lunch and 1/2 of a sweet potato with dinner.
Black Beans
Bulgur
Butternut squash
Farro
Kidney Beans
Millet
Northern Beans
Potato
Pumpkin
Quinoa
Rice
Sweet potato
Choose fruits with a low glycemic load. People react differently to fruit in their diet so pay attention to how you feel and eat more or less fruit accordingly.
Apple
Apricot
Blueberry
Cantaloupe
Cherry
Grape
Grapefruit
Guava
Kiwi fruit
Lemon
Lime
Mango
Nectarine
Orange
Peach
Pear
Pineapple
Plum
Strawberry
Watermelon